Explore Our Wellness Blog

Da Huang known in Western herbalism as rhubarb root is one of the most potent and respected herbs in Traditional Chinese Medicine (TCM). Classified as a purgative herb, Da Huang is famous for its ability to clear heat, drain dampness, and move stagnation—making it a cornerstone in many classic Chinese herbal formulas. In TCM, Da Huang is bitter and cold in nature, entering the Stomach, Large Intestine, Liver, and Heart meridians. Its primary function is to promote bowel movements by clearing excess heat and accumulation in the digestive tract. For patients suffering from constipation due to heat, dehydration, or stagnation, Da Huang can be highly effective when used appropriately. Unlike simple laxatives, it addresses the underlying energetic imbalance rather than just the symptom. Beyond digestion, Da Huang is also used to clear heat from the blood, reduce inflammation, and break up blood stasis. This makes it valuable in formulas for conditions such as skin eruptions, abscesses, menstrual pain with clotting, and certain acute inflammatory disorders. Modern research has identified compounds such as anthraquinones, which contribute to its laxative and anti-inflammatory effects. However, Da Huang must be used with precision and professional guidance. Because of its strong downward-moving action, it is not appropriate for patients who are weak, deficient, pregnant, or suffering from chronic loose stools. In clinical practice, TCM practitioners and herbalists often modify the dosage or combine Da Huang with other herbs to balance its effects and protect the digestive system. Da Huang exemplifies the sophistication of Chinese herbal medicine—powerful, targeted, and highly effective when prescribed by a trained practitioner. When used correctly, it can restore balance, relieve stagnation, and support healthy digestion and circulation. Dr. Ajay Purohit DTCM spectrumwellcare@gmail.com 407-347-5038
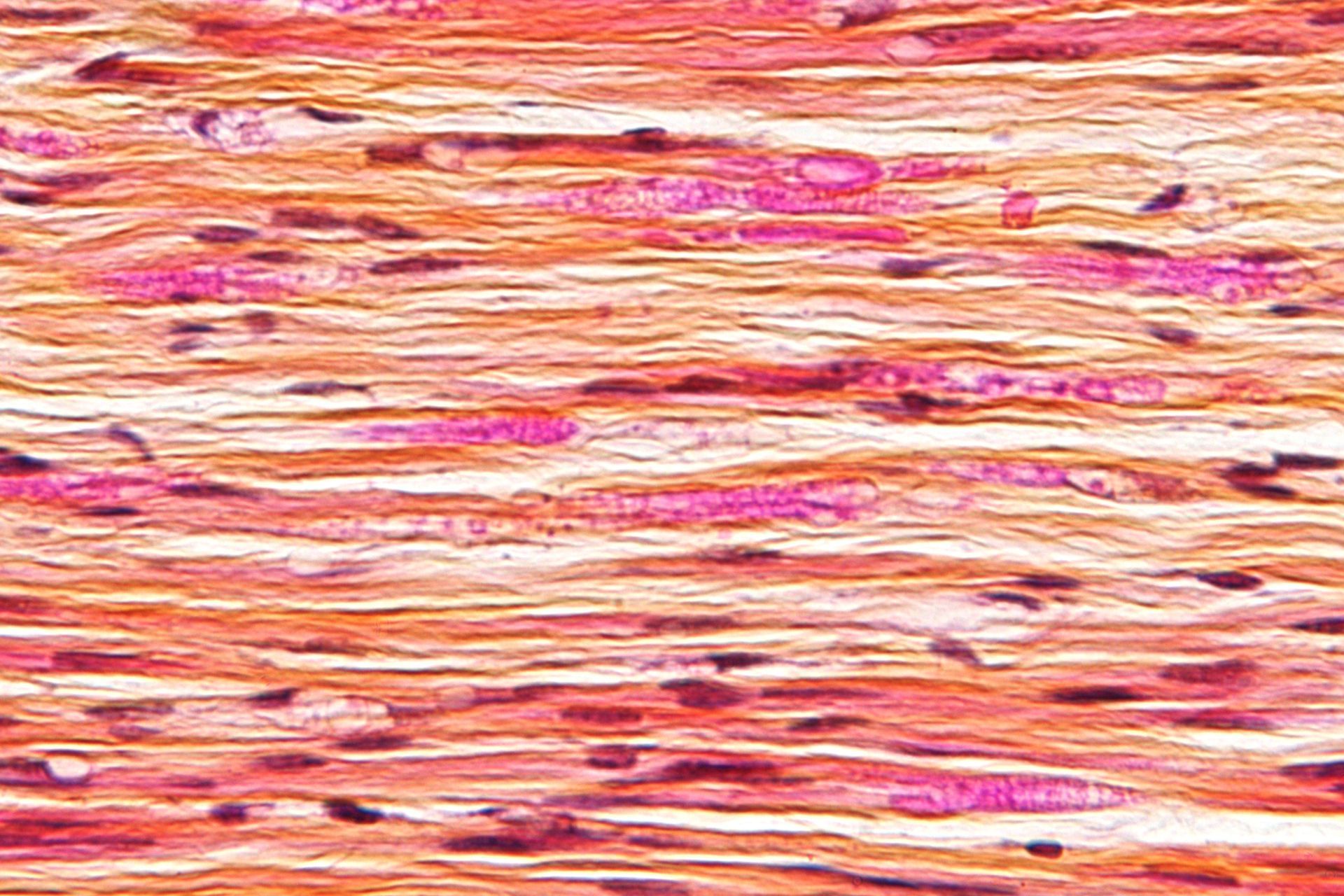
Nerve impingement, often called a “pinched nerve,” occurs when surrounding tissues—such as muscles, tendons, bones, or discs—place excessive pressure on a nerve. This pressure disrupts normal nerve function and can lead to pain, numbness, tingling, or weakness along the nerve’s pathway. Common areas affected include the neck, lower back, shoulders, and wrists. There are several causes of nerve impingement. Poor posture, repetitive movements, spinal disc degeneration, herniated discs, arthritis, and muscle tension are frequent contributors. In the lower back, nerve impingement can result in sciatica, causing pain that radiates down the leg. In the neck, it may produce symptoms that travel into the shoulder, arm, or hand. Symptoms vary depending on the location and severity of the impingement. Some people experience sharp or burning pain, while others notice dull aches, muscle weakness, or a “pins and needles” sensation. Left untreated, chronic nerve compression can lead to long-term nerve irritation and decreased function. Conventional treatment options often include rest, anti-inflammatory medications, physical therapy, or injections. While these approaches may provide relief, many patients seek natural, drug-free options to address both pain and underlying tension patterns. Acupuncture with MPS Therapy offers a holistic approach to nerve impingement by improving circulation, reducing inflammation, and relaxing tight muscles that may be compressing nerves. By targeting specific acupuncture points, treatment helps calm the nervous system and promote the body’s natural healing response. Many patients also notice improved mobility and reduced pain after consistent care. If you’re experiencing persistent nerve pain, early intervention is key. Addressing nerve impingement naturally can help prevent progression and support long-term nerve health and overall well-being. Dr. Ajay Purohit DTCM spectrumwellcare@gmail.com 507-347-5038
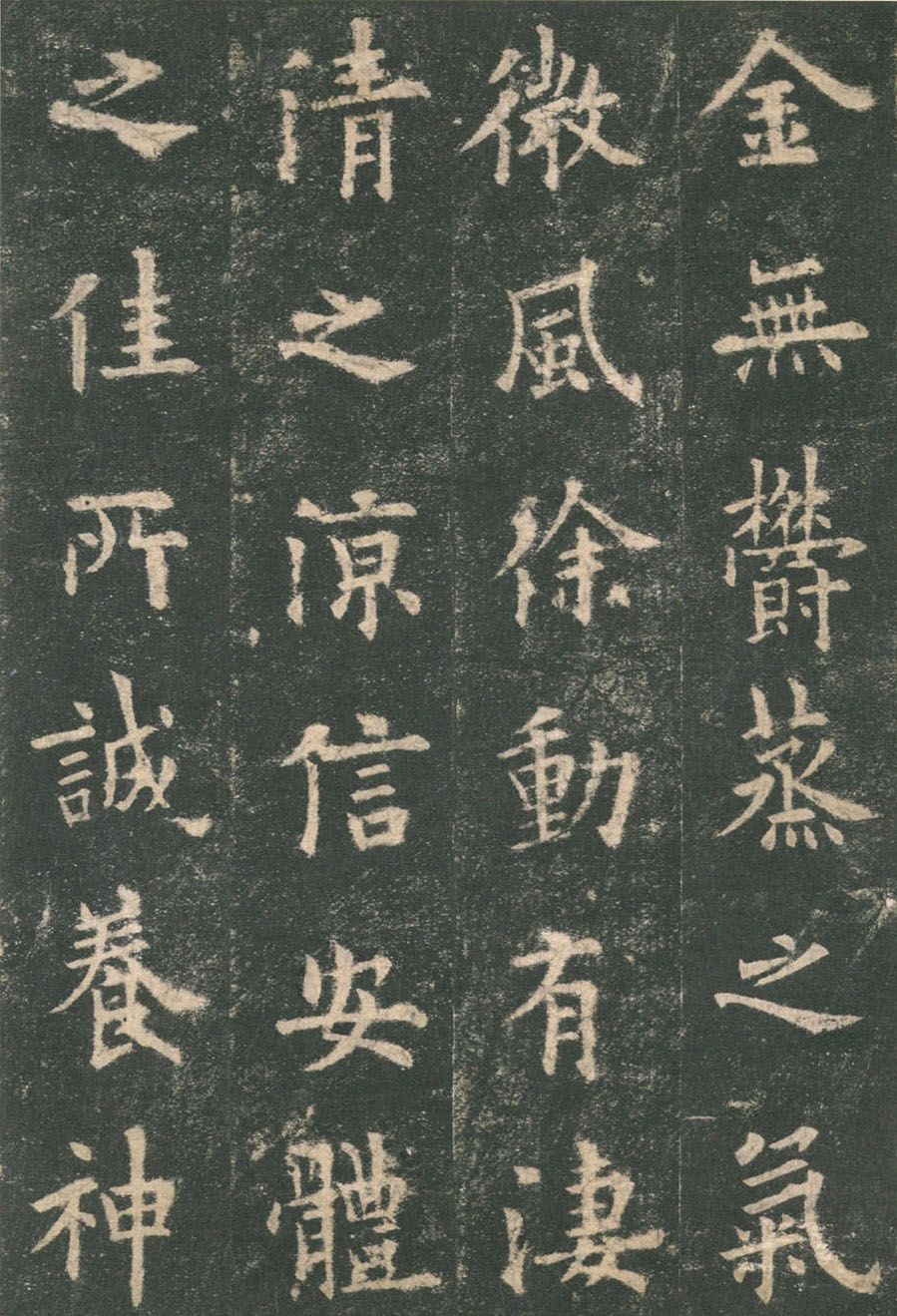
The Ben Cao Gang Mu, translated as Compendium of Materia Medica, is one of the most influential medical texts in the history of Traditional Chinese Medicine (TCM). Compiled by the renowned Ming Dynasty physician Li Shi-Zhen (1518–1593), this monumental work represents the culmination of centuries of herbal knowledge and clinical observation. Completed after nearly 30 years of research, the Ben Cao Gang Mu systematically documents 1,892 medicinal substances, including herbs, minerals, and animal products. It also records over 11,000 prescriptions, making it far more than a simple herbal list. Li Shi-Zhen critically reviewed earlier materia medica texts, corrected errors, clarified herb identification, and added extensive clinical commentary based on direct experience. One of the most important contributions of the Ben Cao Gang Mu is its organized classification system. Herbs are grouped according to natural categories rather than purely therapeutic actions, reflecting a deep understanding of nature and its relationship to the human body. Each entry includes information on taste, temperature, meridian affiliation, functions, indications, preparation methods, and cautions—principles that still guide herbal prescribing today. From a modern clinical perspective, the Ben Cao Gang Mu exemplifies evidence-based practice within a traditional framework. Li Shi-Zhen emphasized observation, safety, and appropriate usage, often warning against misuse or overreliance on potent substances. His work bridges philosophy, medicine, and natural science, influencing not only Chinese medicine but also pharmacology, botany, and zoology worldwide. For today’s acupuncturists and herbalists, the Ben Cao Gang Mu remains a foundational reference. While contemporary practice often relies on modern textbooks and standardized formulas, this classic reminds us of the roots of herbal medicine: careful study, respect for nature, and individualized treatment. Understanding the Ben Cao Gang Mu deepens clinical insight and strengthens our connection to the rich lineage of Traditional Chinese Medicine. Dr. Ajay Purohit DTCM spectrumwellcare@gmail.com 407-347-5038

Gallbladder 34 (GB34), known as Yanglingquan or the “Yang Mound Spring,” is one of the most important acupuncture points in Traditional Chinese Medicine. Located just below the lateral aspect of the knee, in a depression anterior and inferior to the head of the fibula, GB34 is revered as the Hui-Meeting Point of the Sinews. This means it has a powerful influence on the tendons, ligaments, and musculoskeletal system, making it a key point for relieving pain, improving mobility, and supporting physical performance. Clinically, GB34 is commonly used to treat conditions involving stiffness, tightness, or weakness of the muscles and joints. It is especially helpful for knee pain, sciatica, hip tightness, leg cramps, and limited range of motion. Athletes and active individuals benefit greatly from this point because it helps promote flexibility, coordination, and muscular resilience. By activating GB34, practitioners encourage the smooth flow of Liver and Gallbladder Qi, which helps release tension and restore balance to the body’s movement channels. Beyond its physical benefits, GB34 also plays an important role in emotional and energetic regulation. In Chinese medicine, the Gallbladder is associated with courage, decision-making, and the ability to move forward in life. When Liver and Gallbladder Qi becomes stagnant, individuals may experience frustration, irritability, or hesitation. Stimulating GB34 helps harmonize these energies, promoting a greater sense of clarity, confidence, and emotional ease. GB34 is also used to support digestive issues, headaches along the lateral head pathway, and disorders of the ribcage and costal region. Its broad range of therapeutic actions makes it a versatile and essential point in many acupuncture treatments. Whether used for pain relief, athletic recovery, emotional balance, or overall health maintenance, Gallbladder 34 exemplifies the holistic wisdom of acupuncture—addressing the body, mind, and energetic pathways together to promote lasting wellness and harmony.

Chuan Xin Lian, known botanically as Andrographis paniculata, is one of the most valued bitter herbs in Traditional Chinese Medicine (TCM). Often called the “King of Bitters,” its strong cooling nature makes it a go-to remedy for clearing heat, resolving toxicity, and supporting the body’s natural defenses. For patients seeking natural approaches to immunity and inflammation, Chuan Xin Lian offers a time-tested solution rooted in centuries of herbal wisdom. In TCM, Chuan Xin Lian enters the Lung, Stomach, Large Intestine, and Small Intestine channels. Its primary actions include clearing heat, drying dampness, and reducing swelling. Practitioners commonly use it for conditions such as sore throat, fever, acute respiratory infections, and digestive discomfort involving heat or damp-heat patterns. Because of its strong bitter and cooling qualities, it helps disperse pathogenic heat while supporting the body’s internal balance. Modern research increasingly highlights Chuan Xin Lian for its antimicrobial, antiviral, and anti-inflammatory properties. Many patients recognize it as an ingredient in popular immune-support herbal blends. When used appropriately, it can shorten the duration of upper respiratory symptoms, ease throat irritation, and support the body during seasonal immune challenges. However, due to its potency, Chuan Xin Lian is not a one-size-fits-all herb. Its intense bitterness and strong cooling nature make proper diagnosis essential. It is best used under the guidance of a licensed acupuncture physician or herbalist, particularly for patients who are constitutionally cold, deficient, or pregnant. For those looking to integrate herbal medicine into their wellness routine, Chuan Xin Lian can be a powerful ally. Whether used alone or combined with other heat-clearing herbs, it embodies the precision and effectiveness of Traditional Chinese Medicine. If you're experiencing symptoms of heat or looking for natural immune support, this herb maybe the right fit for your needs. Dr. Ajay Purohit DTCM spectrumwellcare@gmail.com 407-347-5038

Bladder 40 (Wei Zhong), located at the midpoint of the popliteal crease behind the knee, is one of the most powerful and clinically essential acupuncture points in Traditional Chinese Medicine. Known as the Command Point of the Lower Back, BL40 has been used for centuries to treat lumbar pain, leg tension, heat conditions, and disorders along the Bladder meridian. In TCM theory, the Bladder channel runs from the inner canthus of the eye, down the back, through the sacrum, and along the posterior legs. Because BL40 sits at a major energetic crossroads, stimulating it strongly influences qi and blood circulation throughout the entire channel. This makes it one of the most dependable points for relieving acute and chronic low back pain, sciatica, stiffness, or injury-related tension. Clinically, BL40 is frequently selected for patients who spend long hours standing, lifting, or sitting—common lifestyle patterns that contribute to lumbar stagnation. Needling or acupressure at this point helps relax the sinews, ease muscle spasms, reduce inflammation, and open the channel to encourage smoother flow. For patients with sciatic pain, BL40 often provides rapid relief because of its deep connection to the hamstrings and lower spine. In addition to musculoskeletal benefits, BL40 is also used to clear internal heat. In classical texts, it is noted for helping with skin conditions like eczema, urticaria, and summer heat symptoms. Its ability to cool and move blood makes it a valuable point for detoxification and promoting overall balance. In modern practice, BL40 can be incorporated into treatment plans for athletes, patients with chronic lumbar issues, or anyone experiencing tension along the Bladder channel. Whether used alone or in combination with points like BL23, GB30, or BL60, it remains a cornerstone of effective acupuncture therapy. For individuals seeking natural relief from low back pain or sciatic discomfort, Bladder 40 continues to shine as one of TCM’s most reliable and transformative points. Dr. Ajay Purohit DTCM spectrumwellcare@gmail.com 407-347-5038

In Traditional Chinese Medicine (TCM), Fu Ling (Poria cocos) is one of the most commonly used and versatile herbs. Known as a “spirit-calming” and “dampness-draining” herb, Fu Ling is a type of medicinal fungus that grows around the roots of pine trees. For thousands of years, it has been valued for its gentle yet powerful effects on the body and mind. From a TCM perspective, Fu Ling works primarily on the Spleen, Heart, and Kidney meridians. It helps to strengthen the Spleen, which in TCM governs digestion and the transformation of food into energy. When the Spleen is weak, symptoms such as fatigue, bloating, loose stools, and water retention can arise. Fu Ling helps to resolve these issues by promoting urination and eliminating excess dampness—a common underlying cause of sluggish digestion and heaviness in the body. Beyond its physical benefits, Fu Ling is also known for its calming and grounding effects on the spirit (Shen). It can help reduce anxiety, restlessness, and insomnia caused by Heart and Spleen disharmony. This makes it an excellent herb for those who feel mentally overworked or emotionally unsettled. Modern research supports some of these traditional uses, showing that Fu Ling has anti-inflammatory, diuretic, and immune-boosting properties. It’s often combined with other herbs such as Bai Zhu (Atractylodes) and Gan Cao (Licorice) to enhance its tonifying effects. Whether used in an herbal formula, tea, or supplement, Fu Ling offers a gentle way to restore balance, improve digestion, and calm the mind. Its subtle yet profound influence makes it a cornerstone herb for promoting overall wellness and harmony in the body—an enduring symbol of TCM’s holistic wisdom. Dr. Ajay Purohit DTCM spectrumwellcare@gmail.com 407-347-5038

In Traditional Chinese Medicine (TCM), few herbs are as well-known and widely respected as Da Huang, also called Rhubarb Root. Known for its strong detoxifying and purging actions, Da Huang has been used for centuries to clear excess heat, eliminate stagnation, and restore balance within the body. Da Huang’s primary function is to clear heat and move the bowels. In TCM theory, when internal heat or toxins accumulate, they can cause constipation, inflammation, or symptoms such as headaches, irritability, and red eyes. Da Huang helps by promoting healthy elimination and supporting the body’s natural detox processes. Because of its potency, it is often used in carefully balanced formulas rather than on its own. Beyond its purgative effects, Da Huang also invigorates blood circulation and removes blood stasis, making it useful in conditions where stagnant blood causes pain or swelling. In modern herbal practice, it may appear in formulas that address menstrual irregularities, skin eruptions, or digestive sluggishness—always in small, harmonized doses. Da Huang is used strategically to “open the gates” and allow the body to release what no longer serves it. When combined with gentler herbs that protect the digestive system, it becomes a tool for transformation rather than harsh cleansing. Because Da Huang is so powerful, it should only be used under the guidance of a qualified practitioner. The right dose and formula depend on each individual’s pattern of imbalance. When prescribed properly, Da Huang exemplifies TCM’s brilliance: using nature’s strength to restore inner harmony. Dr. Ajay Purohit DTCM spectrumwellcare@gmail.com 407-347-5038

In Traditional Chinese Medicine (TCM), acupuncture points are often paired together to enhance their therapeutic effects. One particularly effective combination is San Jiao 5 (Waiguan) and Gallbladder 40 (Qiuxu). This duo is commonly used to harmonize the body’s internal and external energies, making it a powerful choice for conditions related to stress, pain, and energy flow. San Jiao 5, located on the outer forearm, is known as the Luo-Connecting point of the San Jiao channel and also a key point for releasing exterior conditions. It helps regulate Qi and clear heat, often used for headaches, neck tension, fevers, and emotional imbalances. By opening the Yang Linking Vessel (Yang Wei Mai), it connects and harmonizes the body’s Yang channels, making it highly effective for overall balance. Gallbladder 40, found just in front of the outer ankle, is the Yuan-Source point of the Gallbladder channel. It helps regulate liver and gallbladder function, alleviates pain along the channel (such as hip, leg, and ankle discomfort), and supports emotional well-being. Because the Gallbladder is closely linked to decision-making and courage in TCM theory, stimulating GB40 can also help release frustration and indecision. When SJ5 and GB40 are combined, they create a strong therapeutic synergy. Together, they address conditions like migraines, dizziness, stress-induced tension, and disorders along the Shaoyang channels (which govern the sides of the body, temples, and ears). This combination not only reduces pain and stiffness but also promotes a smoother flow of Qi, supporting both physical relaxation and emotional clarity. By harmonizing external defenses with internal balance, the SJ5–GB40 pairing exemplifies the wisdom of TCM point combinations: simple yet profound in restoring health and harmony. Dr. Ajay Purohit DTCM spectrumwellcare@gmail.com 407-347-5038

In Traditional Chinese Medicine (TCM), Da Huang, also known as rhubarb root, is one of the most important and widely used herbs in the materia medica. Belonging to the category of herbs that drain downward, Da Huang is best known for its strong purgative action, helping to clear excess heat and stagnation from the body. Da Huang is particularly effective in addressing conditions of constipation caused by heat accumulation. By promoting bowel movements, it helps release toxins, reduce internal fire, and restore balance. Beyond its laxative effect, it also cools the blood, dispels blood stasis, and clears damp-heat, making it useful in treating a wide range of conditions such as infections, inflammation, or even traumatic injuries with swelling and pain. One of the unique aspects of Da Huang is its ability to both purge and invigorate. When prepared raw, it has a strong downward-draining action. However, when cooked or wine-processed, its focus shifts toward moving blood and relieving stasis. This versatility allows practitioners to tailor its use based on the patient’s needs. Modern research supports Da Huang’s traditional functions, noting its anti-inflammatory, antibacterial, and liver-protective properties. It has been studied for its role in supporting digestive health, detoxification, and even cardiovascular function. Because of its potency, Da Huang must be prescribed with caution. It is not suitable for those with weakness, chronic digestive disorders, or during pregnancy. In clinical practice, it is almost always combined with other herbs to moderate its intensity and guide its effects. In short, Da Huang is a powerful herb that embodies the TCM principle of restoring harmony by clearing excess. When used skillfully, it provides profound relief and healing. Dr. Ajay Purohit DTCM spectrumwellcare@gmail.com 407-347-5038






